Urgent care billing is a critical operational function for urgent care centers managing high patient volumes, short visit durations, and diverse payer requirements. Accurate billing processes directly affect reimbursement speed, revenue stability, and compliance. Due to the fast-paced nature of urgent care settings, billing errors, documentation gaps, and coding mistakes can quickly lead to claim denials and revenue loss.
This article explains urgent care billing, urgent care billing services, Urgent Care RCM, urgent care EHR, Urgent Care Revenue Cycle Management, and urgent care CPT coding in a clear, professional manner.
What Is Urgent Care Billing
Urgent care billing refers to the process of capturing services provided during urgent care visits, assigning appropriate medical codes, submitting claims to payers, and collecting payments. Unlike traditional physician practices, urgent care centers handle walk-in patients, extended hours, varied acuity levels, and a wide range of services.
Effective urgent care billing requires precise documentation, accurate coding, timely claim submission, and continuous follow-up to ensure correct reimbursement.
Importance of Urgent Care Billing Services
Urgent care billing services support healthcare organizations by managing billing workflows efficiently and compliantly. These services help urgent care centers reduce administrative burden and focus on patient care.
Professional urgent care billing services improve claim accuracy, ensure payer guideline adherence, and streamline reimbursement cycles. With specialized expertise in urgent care operations, billing services address common challenges such as eligibility issues, coding errors, and denial management.
Core Components of Urgent Care Billing Services
Urgent care billing services include several essential processes that ensure financial performance.
Eligibility verification
Insurance verification before treatment minimizes coverage-related denials.
Charge capture
Accurate capture of all services ensures no revenue leakage.
Coding validation
Claims are reviewed to confirm proper code assignment and compliance.
Claim submission
Clean claims are submitted promptly to reduce payment delays.
Denial management
Denied claims are analyzed, corrected, and resubmitted efficiently.
Role of Urgent Care EHR in Billing Accuracy
Urgent care EHR systems play a major role in billing success. Proper EHR usage ensures that clinical documentation supports accurate coding and claim submission.
Structured templates within urgent care EHR guide providers to document required elements such as history, examination, and medical decision-making. Automated prompts improve documentation completeness and consistency.
Integration between urgent care EHR and billing systems reduces manual data entry, improves data accuracy, and accelerates claim submission timelines.
Understanding Urgent Care Revenue Cycle Management
Urgent Care Revenue Cycle Management encompasses the financial process from patient registration to final payment collection. Effective Urgent Care RCM ensures stable cash flow and operational efficiency.
Urgent Care Revenue Cycle Management focuses on proactive eligibility checks, accurate coding, timely billing, denial resolution, and payment reconciliation. Each stage of the cycle contributes to overall revenue performance.
Key Stages of Urgent Care RCM
Patient access and registration
Accurate demographic and insurance data collection supports clean claims.
Eligibility verification
Verification reduces rejected claims related to inactive coverage.
Coding and charge capture
Proper documentation supports correct code assignment.
Claim submission
Timely submission improves reimbursement turnaround.
Denial follow-up
Effective follow-up recovers lost revenue.
Payment posting
Accurate posting ensures financial transparency.
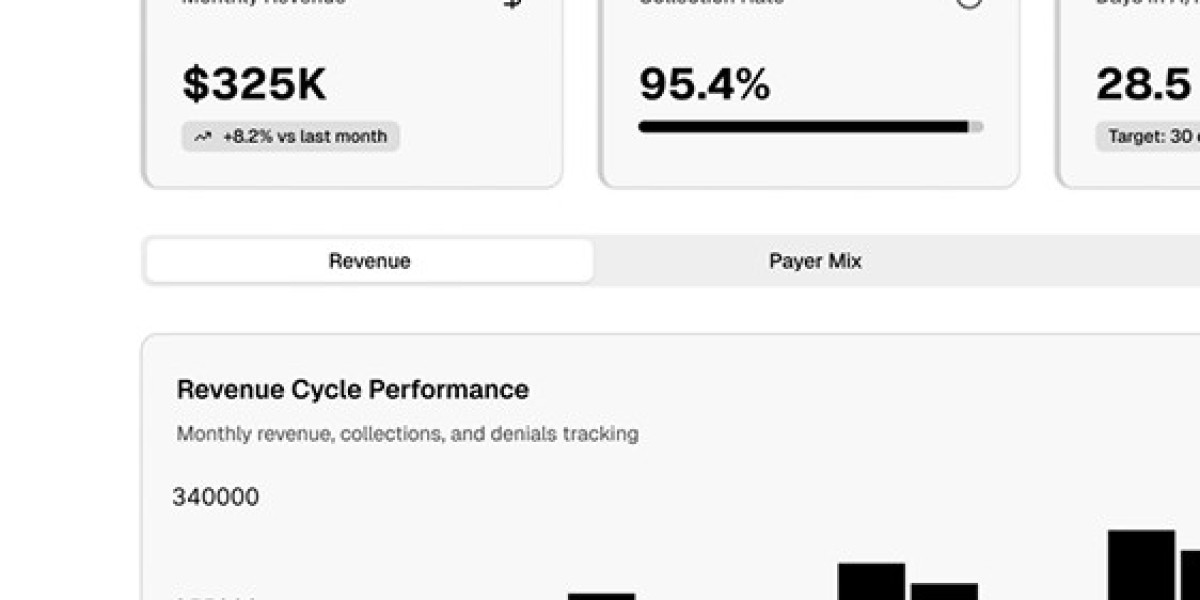
How Urgent Care RCM Improves Financial Performance
Urgent Care RCM reduces claim rejections by ensuring coding accuracy and documentation compliance. Continuous monitoring of key performance indicators such as denial rates and accounts receivable days improves revenue predictability.
Urgent Care RCM also supports scalability, allowing urgent care centers to manage growth without compromising financial controls.
Importance of Urgent Care CPT Coding
Urgent care CPT coding defines how services provided during visits are billed to payers. Accurate CPT coding reflects visit complexity, procedures performed, and provider effort.
Urgent care visits often involve evaluation and management services, diagnostic tests, minor procedures, and treatments. Correct CPT coding ensures appropriate reimbursement while maintaining compliance.
Common CPT Codes Used in Urgent Care
Evaluation and Management codes (99202–99215)
Used based on medical decision-making or time.
Procedure codes
Include wound care, laceration repair, injections, and splinting.
Diagnostic services
Laboratory tests and imaging require proper coding alignment.
Preventing Denials Through Accurate CPT Coding
Urgent care CPT coding errors often result from incomplete documentation or incorrect modifier usage. Accurate documentation supports code selection and reduces audit risks.
Modifiers clarify special circumstances and help avoid payer rejections. Consistent coding audits ensure ongoing compliance.
Choosing the Right Urgent Care Billing Company
Selecting an experienced urgent care billing company is essential for long-term success. A reliable billing partner understands urgent care workflows, payer policies, and compliance requirements.
Key factors to consider include certified coding professionals, technology integration with urgent care EHR systems, proven urgent care experience, and transparent reporting.
Future Trends in Urgent Care Billing and RCM
Technology continues to shape urgent care billing processes. Automation, artificial intelligence, and real-time analytics improve coding accuracy and billing efficiency.
Integrated urgent care EHR platforms combined with advanced Urgent Care Revenue Cycle Management tools provide real-time visibility into financial performance, enabling proactive decision-making.
Conclusion
Urgent care billing requires precision, efficiency, and compliance to ensure financial stability. Professional urgent care billing services, effective Urgent Care RCM, optimized urgent care EHR usage, and accurate urgent care CPT coding work together to reduce denials and improve reimbursement outcomes. Investing in structured billing processes and experienced partners helps urgent care centers maintain profitability while delivering quality patient care.